Prescription Drug Benefits
Announcement
Looking for 2026 Open Enrollment information? Please visit our new 2026 Open Enrollment page for the latest updates, resources, and important dates.
All four Northwestern-sponsored medical plans provide benefits toward the cost of prescription drugs. Express Scripts is the Pharmacy Benefit Manager for all four plans. If you have questions about a covered medication, contact Express Scripts directly at (800) 601-9314 with identification number K9EA.
You can price medications, do a formulary look up, find participating pharmacies, and review plan highlights on the Express Scripts website.
- Copays
- Generics preferred
- If you are prescribed a specialty drug
- Smart90: Required 90-Day Supply
- SaveOn SP
- GLP-1 Drugs: EnGuide Pharmacy
- Price A Medication
- Claim forms
Copays
Retail, one month supply
| Premier PPO, Select PPO and HMO Illinois | Value PPO |
|---|---|
|
You pay a copay of:
|
|
|
Other Considerations |
|
|
Premier PPO, Select PPO and HMO Illinois |
Value PPO |
|
|
| Certain drugs have per month or benefit period limits, step therapy requirements, or prior authorization. Contact ExpressScripts or check with your pharmacist or physician for a list of drugs subject to limitations. | |
Home delivery, three month supply
| Premier PPO, Select PPO and HMO Illinois | Value PPO |
|---|---|
|
You pay a copay of:
|
|
|
Other Considerations |
|
|
Premier PPO, Select PPO and HMO Illinois |
Value PPO |
|
|
| Certain drugs have per month or benefit period limits, step therapy requirements, or prior authorization. Contact ExpressScripts or check with your pharmacist or physician for a list of drugs subject to limitations. | |
Generics preferred
Under this program, if a brand-name drug is dispensed rather than an available chemically- equivalent generic drug, an ancillary charge is applied in addition to the member’s generic coinsurance. Ancillary charges are the responsibility of the employee, regardless of whether the “Dispense as Written” box is checked by your doctor. The ancillary charge is 50% of the difference in cost between the brand and generic product. Ancillary charges do not apply towards the maximum cost per prescription or the $1,500 per person out-of-pocket maximum. It is important to remember that this program still allows you the choice between treatment options but not at an increased cost to the plan and its participants.
If you have questions about the ancillary charge for a particular brand medication you are prescribed, contact ExpressScripts.
*Please note that Prior Authorization may be required for certain medications. When you are prescribed one of these medications, your physician will be consulted. The Prior Authorization telephone number is 1-800-417-1764. Provide this number to your physician if a Prior Authorization is required for your medication.
If you are prescribed a specialty drug
Prescriptions for all Specialty Drugs must be filled through Accredo mail order. They cannot be filled at a retail pharmacy, in your provider's office, or at the treatment facility.
Accredo – a wholly owned subsidiary of Express Scripts – is a mail-order pharmacy whose sole purpose is specialty medication management. Accredo fills prescriptions for Specialty Drugs for oral, injectable, and infused medications and provides on-call nurse and pharmacist support for patients on these complex, expensive drugs.
Because many Specialty Drugs require refrigeration, Accredo takes precautions to ensure product preservation, including using temperature-controlled packaging and working with patients to arrange for safe and secure package delivery. For example, if you are unable to receive your medications at home, you may request delivery to your workplace, your doctor’s office, or a family member’s home.
Smart90: Required 90-Day Supply
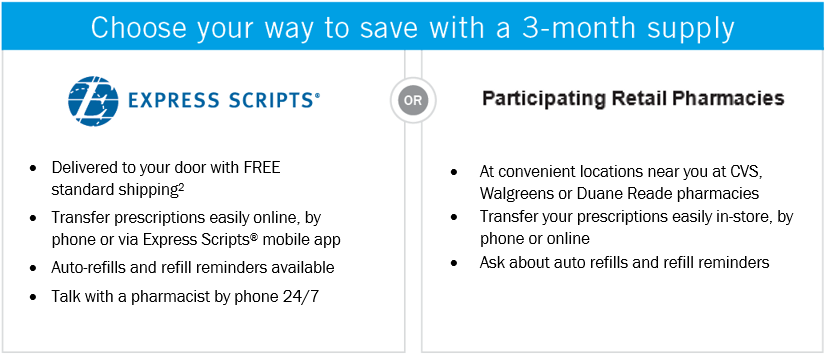
This program will apply to select long-term medications, which will now require a 90-day supply. With Smart90, you can conveniently fill these prescriptions with a 90-day supply either through home delivery from the Express Scripts Pharmacy or from any CVS, Walgreens or Duane Reade pharmacies.
If you keep filling a 1-month supply of the listed long-term medications at a nonparticipating pharmacy, you could pay more. For example, if a drug costs $75, even if your copay or coinsurance is only $20, you could pay up to the full $75. Additionally, when you pay the full cost on retail maintenance medications, your cost share will not count towards you deductible and or maximum out of pocket costs.
What If You Do Not Switch to a 3-Month Supply
Filling a 3-month supply of your long-term medication can help you save time, money and trips to the pharmacy. If you keep filling a 1-month supply at a nonparticipating pharmacy, you could pay more. For example, if a drug costs $75, even if your copay or coinsurance is only $20, you could pay up to the full $75.
SaveOn SP
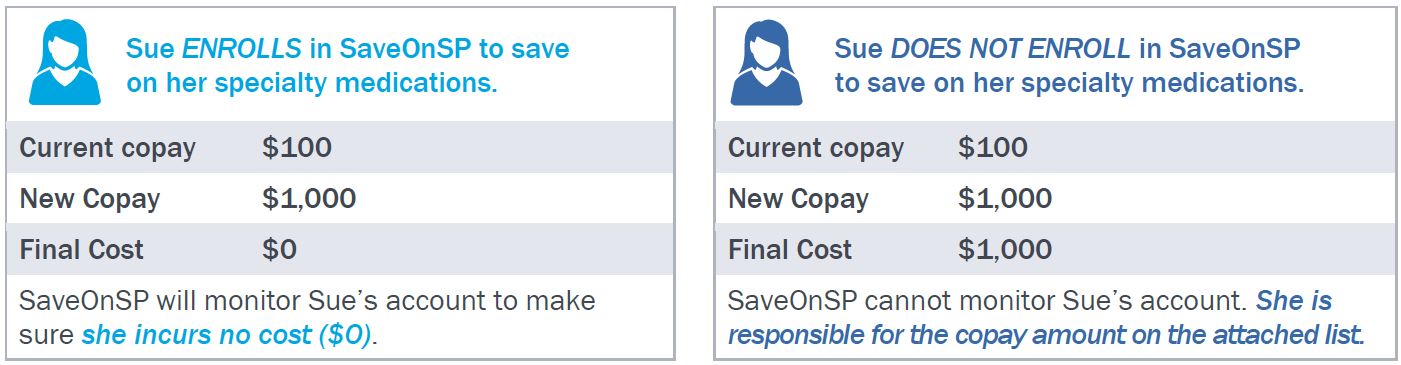
Express Scripts’ program SaveOnSP is designed to help you save money on certain specialty medications for those taking a medication on the SaveOnSP Drug list, and are eligible for the program. Note that the Value PPO is not subject to the SaveOnSP program.- If your specialty medication is noted on the 2025 SaveOn SP Drug List you must participate in the SaveOnSP program to receive your medications free of charge ($0).
- Your prescriptions will still be filled through Accredo, your current specialty pharmacy.
- If you do not participate in the SaveOnSP program, you will be responsible for the copay listed on the attached SaveOnSP Drug list.
- These medications will not count towards your deductible or out-of-pocket maximums.
Contact SaveOnSP at 1-800-683-1074 with questions about eligibility and enrollment.
GLP-1 Drugs: EnGuide Pharmacy
ExpressScripts, Northwestern’s pharmacy benefit for faculty and staff, will launch a new program, EnGuide, to support those prescribed GLP-1 drugs on June 15, 2025. EnGuide was created to expand mail order availability, provide a high-touch support model at pharmacies or by phone, and ensure available supply.
For those filling GLP-1 drugs thorough ExpressScripts, you will receive a letter with instructions on how to move your script to their new EnGuide pharmacy. Those filling scripts at retail pharmacies, such as Walgreen’s or Costco, may continue to use your current pharmacy and will receive a letter outlining access to clinical support through the program. See examples of the member experience for more information on how the program works. For questions, contact Express Scripts at 800-601-9314.
Price A Medication
Use ExpressScripts online pricing tool to price current or future medications. Shopping around may save you money.